Complex coronary intervention refers to the advanced techniques and technologies used by interventional cardiologists to open blocked arteries, which in turn, produce more successful results that were previously unattainable. This is necessary for patients with coronary artery disease that cannot be treated through minimally invasive methods. Historically, such patients were often referred for open-heart surgery. As the population ages and patients become frailer, many are no longer suitable candidates for open-heart surgery. The introduction of new technologies now allows for effective, long-term treatment of complex coronary disease in these patients, significantly improving their quality of life.
Managing High-Risk PCI to Help Clear a Path for Life-Saving Liver Transplantation
A 62-year-old male with a history of coronary artery disease was admitted to Emory University Hospital with end-stage decompensated liver disease. His condition was critical, characterized by refractory ascites, hypotension and coagulopathy, indicating severe hepatic dysfunction. The patient was a candidate for liver transplantation, but the United Network for Organ Sharing (UNOS) required revascularization of a chronically occluded coronary artery, identified as Chronic Total Occlusion (CTO), prior to listing him for transplantation.
Treatment Strategy
Percutaneous Coronary Intervention (PCI) was indicated to revascularize the occluded artery. PCI involves the insertion of catheters through arterial access points, typically in the radial or femoral arteries, advancing to the coronary arteries to relieve the obstruction and deploy a stent to maintain vessel patency. CTOs represent a particularly challenging subset of coronary artery disease, necessitating advanced skill and experience that only a select few operators have in the United States. Given the patient's end-stage liver disease, coagulopathy, and hypotension, he was deemed exceptionally high-risk for the procedure.
Despite the significant risks, the interdisciplinary team at Emory University Hospital, possessing specialized expertise in CTO interventions, proceeded with the PCI. The procedure was performed successfully in the cardiac catheterization laboratory. Following the PCI, the patient was cleared for liver transplantation.
Post-Procedure Follow-up
The patient subsequently underwent a successful liver transplant at Emory Healthcare. At recent follow-up, the patient demonstrated substantial clinical improvement, reporting excellent functional status and quality of life, with the ability to engage in activities such as spending time on his farm with his granddaughter.
Treating Complex Heart Condition After Another Hospital Said No
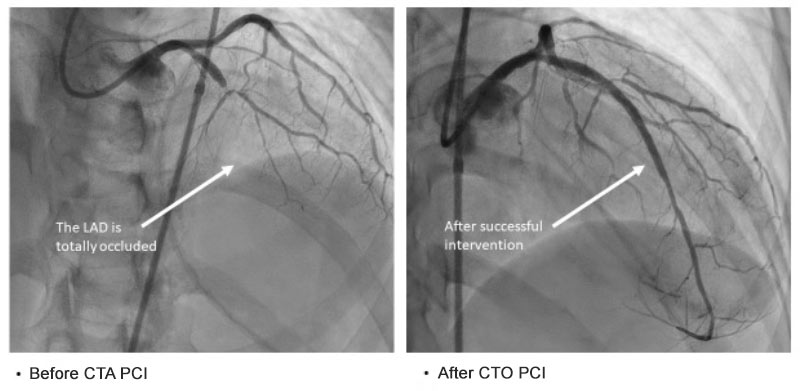
A 55-year-old female initially presented to an outside hospital with new onset heart failure, causing fluid to accumulate in her lungs. Diagnostic workup revealed a total occlusion of the left anterior descending (LAD) artery, which supplies a substantial portion of her heart.
Treatment Strategy
The outside hospital team determined that Percutaneous Coronary Intervention (PCI) to revascularize the occluded LAD was not feasible, deeming it high-risk and unlikely to succeed. Consequently, the patient was discharged with guideline-directed medical therapy (GDMT) for heart failure management.
Seeking a second opinion, the patient presented to Emory University Hospital, where she was evaluated by our interventional cardiology team. After a thorough assessment, it was concluded that PCI was indeed a viable option. Emory's team is equipped with specialized expertise in managing complex coronary interventions, including Chronic Total Occlusions (CTOs).