Why should I take the vaccine if the COVID mortality rate is relatively low?
The death rate for COVID-19 is currently estimated at almost 2% overall, with significant differences based on age groups and medical conditions. However, with so many people infected, even a 2% mortality rate means hundreds of thousands of deaths, including people who are our family, friends and neighbors. Another way to look at it: The population of the United States is 331 million people. So, if everyone in the country became infected with COVID-19, roughly 6 million individuals would lose their life to the virus.
The United States continues to reach grim milestones, with more than 400,000 people who have died from COVID-19 as of January 20, 2021. As a comparison, deaths from the flu during the 2019-2020 flu season were estimated by the CDC to be roughly 22,000.
The vaccine and continued public health efforts (physical distancing, mask wearing, good hand hygiene) help to slow the spread of the virus and prevent deaths.
What are the ingredients in the COVID-19 vaccines?
The Pfizer-BioNTech and Moderna vaccines both contain mRNA, lipids (fats) that help the mRNA to get where it needs to be, and salts and sugars to keep the vaccine stable. The exact formulations are slightly different:
Pfizer-BioNTech COVID-19 Ingredients
- mRNA – The instructions to help your body make a copy of the COVID-19 spike protein, so that your immune system learns to recognize it and make antibodies
- Lipids – Lipids are fats that help protect the mRNA and help it get into cells in the body
- ((4-hydroxybutyl)azanediyl)bis(hexane-6,1-diyl)bis(2-hexyldecanoate)
- 2 [(polyethylene glycol)-2000]-N, N-ditetradecylacetamide
- 1,2-Distearoyl-sn-glycero-3-phosphocholine
- Cholesterol
- Salts – Salts help balance the acidity in your body
- Potassium chloride
- Monobasic potassium phosphate
- Sodium chloride
- Dibasic sodium phosphate dihydrate
- Sucrose – Sugar helps the molecules maintain their shape during freezing and shipping
Read more about the Pfizer-BioNTech COVID-19 vaccine.
Moderna COVID-19 Vaccine Ingredients
- mRNA
- Lipids
- SM-102
- Polyethylene glycol [PEG] 2000 dimyristoyl glycerol [DMG]
- Cholesterol
- 1,2-Distearoyl-sn-glycero-3-phosphocholine [DSPC]
- Ingredients to help stabilize and protect the vaccine during freezing and distribution
- Acetic acid
- Tromethamine & Tromethamine hydrochloride
- Sodium acetate
- Sucrose
Read more about the Moderna COVID-19 vaccine.
Do either of the COVID-19 vaccines contain sulfa?
No, the COVID-19 vaccines do not contain sulfa, as referenced in the complete ingredient list above.
How do I know if I’m allergic to the ingredients in the COVID-19 vaccines?
Severe allergic reactions to the COVID-19 vaccines are rare. A report from the CDC found that the risk of developing a serious allergic reaction is 0.001 percent, based on currently available data.
Rarely, instances of severe allergic reactions have been reported among people immediately following the shot. These are extremely uncommon, with an estimated 11 anaphylactic reactions per million people vaccinated, and are treatable if they occur.
If you have a history of an allergic reaction to any of the listed ingredients, to polyethylene glycol (PEG), or to polysorbate, the CDC recommends that you DO NOT get an mRNA COVID-19 vaccine.
Otherwise, you can likely proceed with vaccination. You should talk to your doctor first if you have experienced a severe allergic reaction from a vaccine or injected medication in the past. The Centers for Disease Control and Prevention (CDC) does recommend that if you have a history of a severe allergic reaction to something else (e.g., oral medications, foods, insects, latex), you can get vaccinated.
Anyone with a history of a severe allergic reaction will be monitored for 30 minutes after vaccination, while all others should be monitored for at least 15 minutes. Vaccination sites have safeguards in place, in the unlikely event you do experience an allergic reaction.
Can you still get COVID-19 after being vaccinated?
Clinical trials of both the Pfizer-BioNTech and Moderna vaccines found a greater than 94% efficacy rate at preventing COVID-19 infection, and almost 100% efficacy at preventing severe infections. These results came after people had received two doses of the vaccine.
While these are very promising results, there are still a very small number of people who may get sick with COVID-19 despite vaccination, and it takes time to complete the vaccine series and develop immunity. We also don’t know whether individuals who have been vaccinated may still be able to shed virus from their noses and mouths and infect others, despite not getting sick themselves. Therefore, it’s important to continue the 3Ws while we work to vaccinate our community:
- Wear your mask
- Wash your hands
- Watch your distance
What is herd immunity?
Herd immunity occurs when a significant portion of the population becomes immune to an infectious disease, so that the disease stops spreading. It can happen by widespread vaccination, or by people developing antibodies after becoming infected with an illness. Because of the risk of serious complications and death from COVID-19, the World Health Organization (WHO) recommends that we achieve herd immunity through vaccinations, NOT by exposure to the virus.
It is difficult to predict when the United States will achieve herd immunity. Experts say that our country needs to have about 200 million immunized or infected citizens to break the chain of infection. (As of January 20, 2021, more than 24 million Americans have been infected with COVID-19. See the country’s latest numbers from the CDC.)
In the meantime, continue wearing a mask, washing your hands and maintaining at least six feet between you and individuals outside of your immediate household. And schedule your vaccination when your phase of eligibility becomes available to you.
Are antibiotics effective at preventing or treating COVID-19?
Antibiotics do not kill the COVID-19 virus. Antibiotics are an effective treatment against infections caused by bacteria, but don’t help to treat or prevent viruses like COVID-19.
Are people who receive the COVID-19 vaccine tracked in any way?
There is nothing within the vaccine itself that would allow anyone to gather your personal information or to track you. The person administering your vaccine doses will record your details in an electronic database for your state – this helps to make sure you get your second dose on the right schedule and that the state gets resupplied with vaccine based on what it has distributed. You will also get a card for your wallet that shows you have been vaccinated.
Is getting the COVID-19 vaccine a bigger risk than contracting the virus?
No, the COVID-19 vaccine is not a bigger risk to your health than becoming ill with the actual virus. COVID-19 can cause many serious short- and long-term symptoms and has killed at least 400,000 Americans, including more than 12,000 right here in Georgia. The COVID-19 vaccine has been proven safe and it is effective at slowing the spread of this very serious virus.
You may experience some side effects after receiving the vaccine. These may include soreness at the injection site, fatigue or fever; however, they are not dangerous and generally go away 24-72 hours later. The COVID-19 virus can trigger symptoms that last days, weeks, or even months.
When you get a COVID-19 vaccine, you’re not just protecting yourself from a potentially deadly virus, you’re also protecting your family, friends and neighbors. Widespread vaccination can also help us return to school and work and enjoy many of the activities we’ve missed over the past year, such as traveling and getting together with friends.
Does the COVID-19 vaccine contain any human tissue, such as fetal cells?
No, there is no human tissue either within the vaccine or used in producing the vaccine. When vaccines contain live virus or pieces of a virus, the virus may need to be grown in a lab, sometimes using human cells. Because these are mRNA vaccines and don’t involve any pieces of the virus, there is no need for that step.
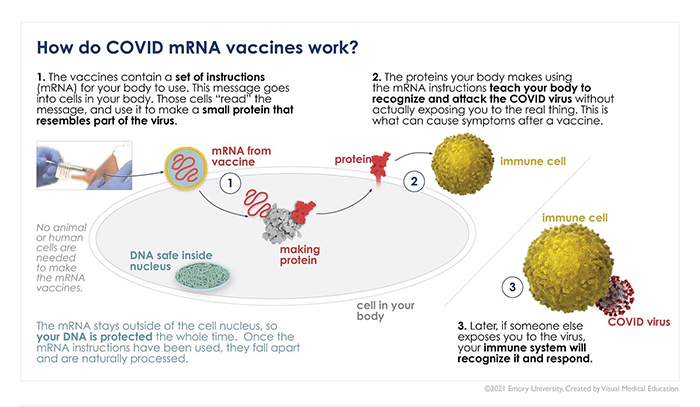
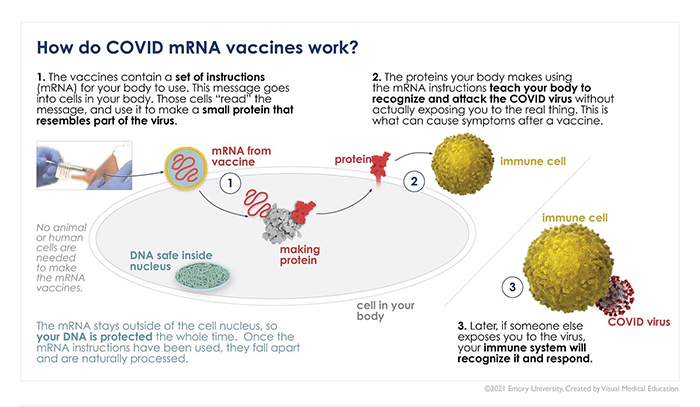
Does the COVID vaccine interact with or alter my DNA?
No, the mRNA in the COVID-19 vaccine does not enter the cell nucleus, which is where your DNA is protected. Once the mRNA enters a cell, its “instructions” are immediately translated to make a copy of the spike protein, which gets cleared out of your body by your immune system as it makes antibodies. The mRNA then disintegrates quickly; it does not stay in your body.
Do I need the vaccine if I’ve had COVID-19?
Yes, you should still get the vaccine even if you’ve been sick with the COVID-19 virus. Researchers are still working to understand how long immunity from the virus lasts. Reinfection is also possible, so the CDC recommends that individuals who have been sick with COVID-19 still receive the vaccine.
Additional resources on COVID-19 and the vaccine
We continue to monitor COVID-19 research developments focused on diagnosing, treating and preventing this very serious public health threat. Our team at Emory Healthcare has compiled helpful resources and answers to your questions to help you take steps to protect you and your loved ones.